Most people don’t need reminding about the cost-of-living crunch: food, petrol, bills and transport all provide a daily reminder that prices are going up. But today’s energy price cap rise – lifting by almost £700 – provides a headline example of the increasing costs of essential goods.. Alongside it, the National Insurance hike (a 2.5 percentage point rise split between employers and employees) and an average council tax rise of 3.5 per cent both kick in too.
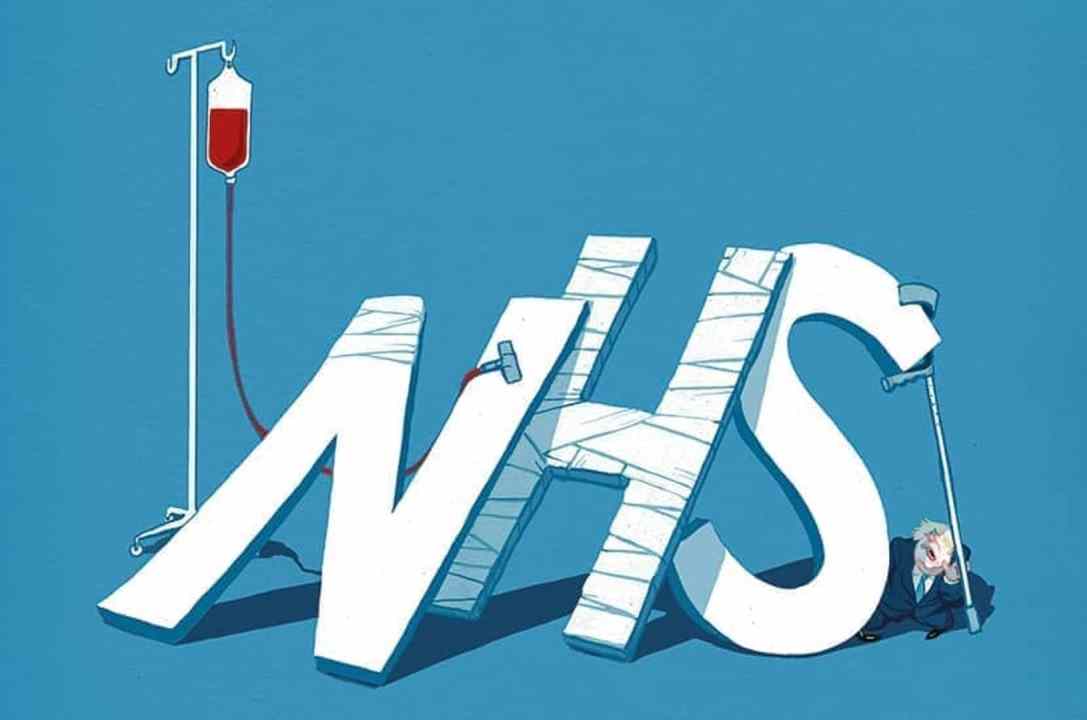
But what about the essential services that are supposedly ‘free’? It seems these are getting expensive too. This week the Private Healthcare Information Network released its data on the number of NHS patients who are paying out of pocket to access private healthcare, due in large part to the long waiting lists (which existed before the pandemic and have worsened since).
Numbers are rising significantly. Nearly 67,100 patients paid to be admitted privately for treatment between July and September 2021, up 35 per cent from pre-pandemic levels. Hip and knee replacements are notably on the rise (up 165 per cent and 122 per cent respectively) as these kinds of operations were quickly cancelled during the heights of the Covid crisis, resulting in some patients waiting for years now, often in pain.
These numbers are reflected in the NHS satisfaction survey released by the British Social Attitudes Survey this week, which found overall satisfaction had fallen by a record-breaking 17 points since 2020, hovering now at just 36 per cent (Isabel Hardman has the details on Coffee House).
So far, there’s little sign of the NHS moving faster to deal with this. As I reported in February, the Covid backlog plan to give more money to the NHS was supposed to include ‘faster diagnosis standards’ for cancer (in which 75 per cent of patients are diagnosed within 28 days) by the end of this year. But when the official recovery plan was announced, this timeline was absent.
At the time, the NHS appeared very close to hitting the 75 per cent target, with the monthly success rate at the end of 2021 above 70 per cent. But numbers have slipped in the most recent update, with the percentage of patients seen within four weeks falling to 64 per cent.
Is the penny starting to drop that the ‘universal access’ promised by the National Health Service isn’t exactly what it says on the tin. For millions of people, universal access’ means a system of rationing, often through waiting lists, keeping them out of hospital and waiting for surgery for months on end? Frustration is only likely to grow over the next few years – the NHS is forecast to get much worse before it gets better, with the internal scenario showing the NHS England waiting list peaking around 9.2 million in March 2024 (closer to 11 million in the downside scenario). This would translate to roughly one in six people in England waiting on their healthcare needs.
People will naturally start seek alternatives. But in Britain – where the independent sector in healthcare is relatively small and has not been incentivised to grow – most people are priced out or will have to make serious financial sacrifices to access it.
It’s a real irony: that a system that purports to offer free access to healthcare for everyone now has skyrocketing numbers of people breaking the bank to pay to avoid it. And all this at a time when inflation is making people feel poorer in every other part of life.







Comments