A research letter in the Future Healthcare Journal, laying out the scale of performance failings in the NHS, has attracted a lot of attention today. It has shone a spotlight on the fact that, to fulfil its pledge to voters to reduce waiting times and ‘fix the NHS’, Labour must somehow find a way to cut the health service’s treatment backlog in half.
The research explains that the NHS has a constitutional requirement that 92 per cent of patients must wait no longer than 18 weeks for treatment after being referred by their GP. That target was last met in November 2015. At that point, the total national waiting list was 3.5 million. By the end of 2024, it was 7.5 million.
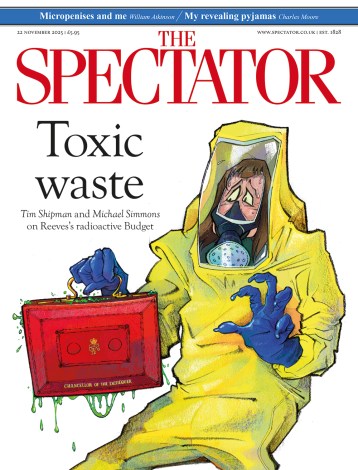
NHS waiting lists are symptomatic of a system that is failing
After much statistical labour – ‘we leverage an equilibrium variant of a mathematical framework previously developed for modelling consultant-led elective waiting times’ – the authors conclude what common sense would have told them to begin with. The list needs to retreat to roughly its 2015 size. But, as a doctor from the Royal College of Physicians of London pointed out, in commenting on the research, the figures represent people living in pain, losing mobility, and slipping into more complex illness as delays accumulate.
Across the political spectrum, there is agreement that the NHS is failing. I have worked on the wards for thirty years, and something has changed in the way I hear people talking about the NHS, a change that would have been unthinkable even a few years ago. Even many of my most left-wing colleagues say bluntly that they feel the NHS, in its current form, is finished and that we need change.
An institution with constitutional requirements it can neither enforce nor meet has lost interest in truthfulness. But when structural rigidity makes real improvements impossible, all that’s left is dishonesty. How might managers achieve lower waiting lists? They have no control over pay and conditions, which are set nationally. They have no ability to reward innovation or hard work, or penalise laziness and indifference. The natural drift in such organisations is towards bloat, not efficiency.
That NHS productivity is bad is no surprise – the real surprise is that it isn’t worse. The fact is that the NHS is full of people who work well and work hard and do so because they genuinely want to help. At the same time, it is also full of those who work badly and as little as possible, and mainly want an easy life, and these two types of people get paid precisely the same.
Care that is free at point of delivery is worth preserving. There are other ways of providing healthcare, and ‘co-pays’ would not mean the end of British civilisation, but free at point of delivery means care can be delivered on the basis of what works rather than what someone can afford. We are right to value that highly. Good medicine is parsimonious – it involves as few tests and as few interventions as possible. A patient wants the minimum intrusion consistent with health; doctors want to deliver exactly that. Currently, NHS doctors have no incentive to inflate clinical work for profit, and the only ones arranging needless interventions are hiding from harder work.
Readers grumbling that the NHS is packed with inefficiency simply have no idea what they’re talking about. You may think it’s bad, but you’re wrong. I work in it, and it’s worse than you can ever imagine. This morning I spent half an hour typing my name, the date, and the time into mandatory pop-ups, all on computers I’d logged into with agonising slowness and that tracked and timed my every keystroke. My colleagues did the same. Waste and abject idiocy are everywhere, at a scale that would rightly bankrupt a private company. Everyone knows that, but no-one can find a way to help. Huge injections of cash haven’t worked, and there’s no reason to think more of them would produce a different result.
Major reorganisations are possible, and studying countries that do better is vital. But major reorganisations don’t come cheap, and Britain’s economy is performing too poorly to allow for grand and expensive experiments.
One solution is simple, though not easy: relax the national rules that prevent different bits of the NHS from trying different strategies. Different contracts, pay scales, and terms – without the presumption of a job for life – would allow for local solutions that made local problems better and which could be copied elsewhere. Radical devolution of power, granting local managers the tools to succeed – and accepting that some won’t – is the only way to avert disaster.
NHS waiting lists are symptomatic of a system that is failing. More money, more centralised constitutional requirements, annual ten-year plans – none of this will help. All of us can see that. Changes that were recently unthinkable need to be embraced without delay. The choice is between planned reconstruction and chaotic collapse. Currently, we’re choosing the latter by default.





Comments