The NHS is in a state of crisis, with increasingly long delays for ambulances and emergency care. Often people believe that hospital delays and bottlenecks are caused entirely by the difficulty of discharging patients to social care. But there is another factor which is just as much of a problem, and which should be far easier to fix: the masses of unnecessary paperwork doctors and nurses have to fill out every day.
In many hospitals as many as 30 pages of nursing documents have to be filled out every time a patient is admitted to hospital
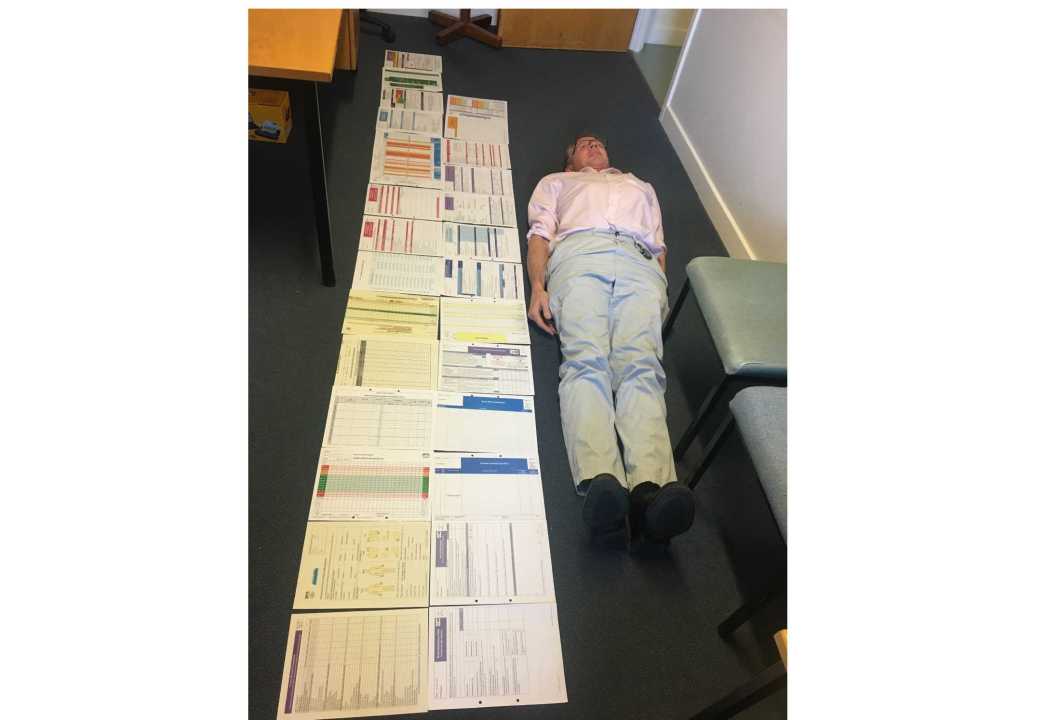
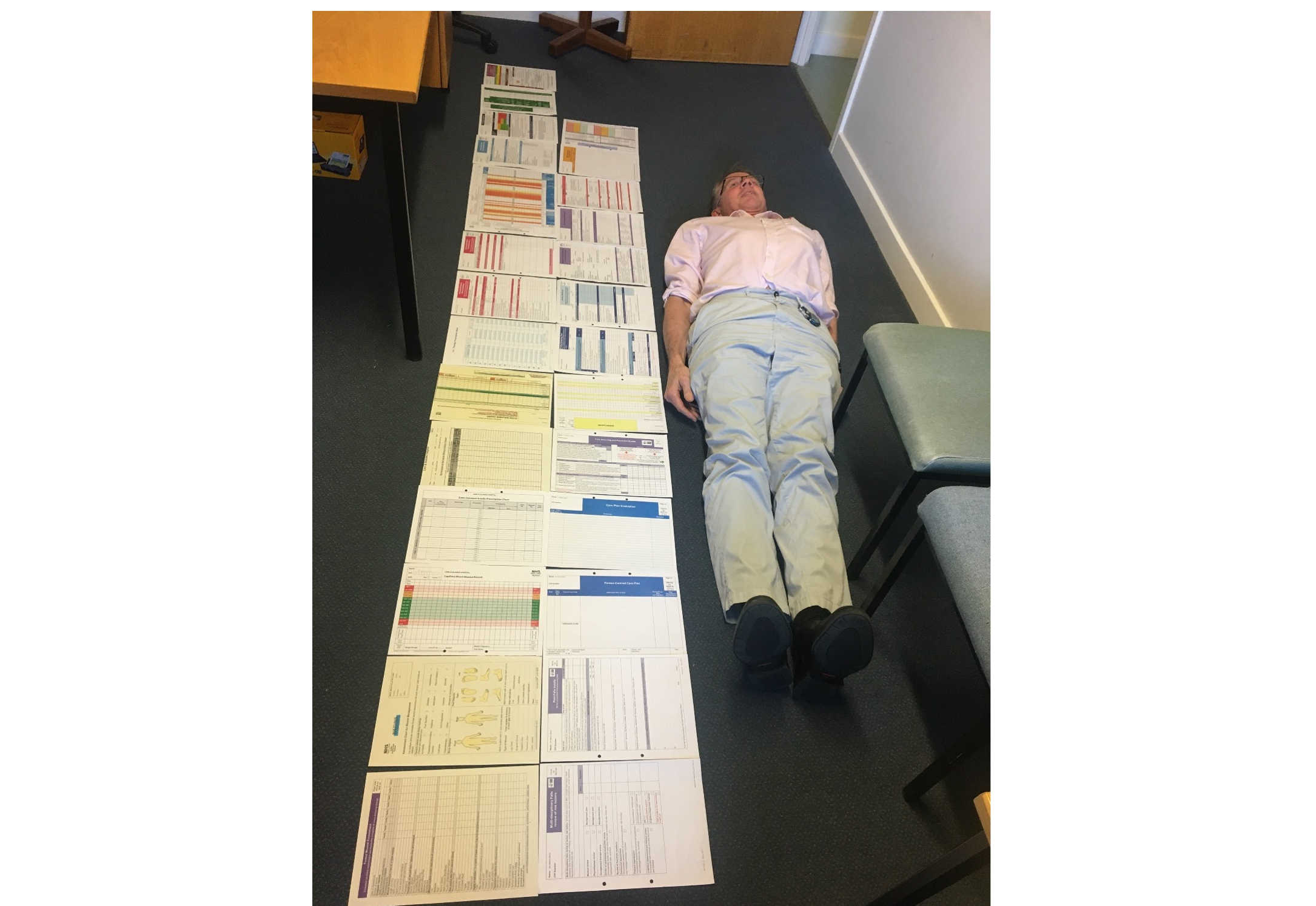
In the picture above, I once laid next to all the forms nurses had to fill out for a single patient who had diabetes and needed intravenous antibiotics. Most of the documents were double sided and there were other forms that had to be filled out on a computer. I am 5ft 10, and I was still dwarfed by the sheer amount of paperwork.
Excessive form filling is the scourge of hospital care. It slows doctors and nurses down, adds little value, and occasionally even undermines or compromises the care we offer.
When I was working as a consultant at Oban Hospital in Scotland, if a patient appeared to have had a mini stroke, the X-ray department required a doctor to complete four request forms by hand, writing identical details on each form. Examining a patient would perhaps only take ten minutes but filling the forms took 20. If the NHS was able to replace this with one form, 15 minutes would be saved for each patient, with no financial cost. This would allow a doctor to see the next patient 15 minutes earlier, and would help the hospital avoid breaching the target for every patient to be seen within four hours. Missing this target means that further paperwork has to be completed, wasting even more time.
In an A&E department, a patient assessment and a decision to discharge would often take as little as ten minutes. But even though I am computer literate, the NHS IT systems were so counter-intuitive that a two-minute discharge letter could take 20 minutes to complete.
All of these forms have not improved safety, productivity or efficiency. If anything they have led to a kind of flawed nursing philosophy that holds that a patient hasn’t been cared for unless there is exhaustive documentation. The prevalent view is that a nurse cannot be defended without paperwork if there is a complaint or legal case.
In many hospitals as many as 30 pages of nursing documents have to be filled out every time a patient is admitted to hospital, with each form requiring patient identification labels. Often the patient’s name, date of birth and NHS number must be handwritten several times, which alone can take 30 minutes before the nurse starts to enter any other information. There is frequent duplication. For example, a patient’s weight may be required on six of the forms and can result in several different weights being recorded. If the patient is readmitted the nurse must start again with new blank forms.
Imagine if the toilets in motorway service stations were run by the NHS. At the moment, in a typical loo you can see when it was last cleaned, who did the work and how to raise a concern. If the NHS model was used there would be a huge cleaner’s checklist, with a separate form for each cubicle, sink and the floors. In each cubicle would be a tick box list: ‘Opened door, lifted toilet seat, picked up the brush’ and so on. In reality, the NHS could learn from these motorway service stations by defining a standard operating procedure, adopting the minimum necessary documentation and putting in place regular supervision.
The nursing hierarchy insists that exhaustive forms are essential for investigating complaints. Incomplete form filling is often used as evidence that nursing staff are not working to a good enough standard, meaning a complaint or legal case is justified. It would be better if the form filling was reduced: many of these bits of paper could be incorporated into a computer template, which would automatically fill-in the patient’s demographics and other details, saving 30 minutes nursing time per admission.
These marginal gains at every step could push forward patient discharges by several hours, enabling hospital to have staffed beds ready for the next day’s arrivals. Patients would be able to move earlier from A&E to the wards, reducing crowding in A&E and waits for ambulances to handover patients.
Another issue is the organisation of our hospital wards. Overcrowding in hospitals often means that patients have to be moved to the wrong wards where there is space for them. This means that consultants have to spend time on ‘Safari Ward rounds’ finding their patients spread across the hospital.This prevents effective team working and communication. In the US and Australia, Dr Jason Stein and nurse Liam Chadwick, reorganised their hospitals so that patients on one ward belonged to a single consultant and their team. This seemingly simple reorganisation along with a type of bedside review ended up reducing a patient’s length of stay in hospital, reduced mortality, lowered readmissions and reduced costs whilst improving patient and staff satisfaction. The NHS could potentially implement this system before next winter.
The NHS has many problems that will be difficult to fix. But reducing the amount of paperwork in the system and reorganising wards would be a relatively simple way to reduce the current strain on the health system. The health service should act now before the next crisis hits.





Comments