Already a subscriber? Log in
This article is for subscribers only
Subscribe today to get 3 months' delivery of the magazine, as well as online and app access, for only £3.
There’s no commitment, you can cancel any time.
- Weekly delivery of the magazine
- Unlimited access to our website and app
- Enjoy Spectator newsletters and podcasts
- Explore our online archive, going back to 1828





Comments
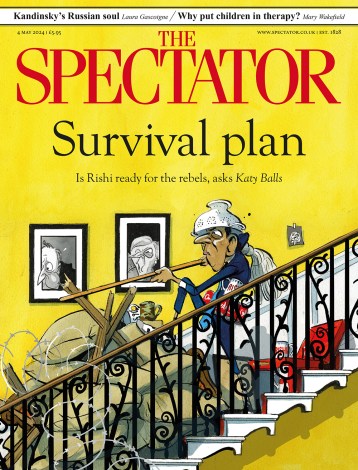
A blooming good offer
Join the conversation with other Spectator readers by getting the next 3 months for £3.
CLAIM OFFER 3 months for £3Already a subscriber? Log in