Embarking on the quest to lose weight can be a risky business. Yo-yo dieting, compulsive binging, muscle wasting and brain fog are just some of the many challenges that have waylaid dieters over the years. But now, thanks to the arrival of seductive weight loss drugs promising a quick fix, calorie counters are facing more contemporary health problems – from extreme discomfort, organ dysfunction and even death. Just this week, an inquest heard that Breeda O’Donoghue, a 66-year-old grandmother from Cork, Ireland passed away from multiple organ failure after taking Ozempic for diabetes and weight loss. But she’s far from the only person who has experienced devastating – and fatal – complications from the drug.
Most often referred to by its brand name Ozempic, this semaglutide medication fascinated the Western world after it emerged that, as well as treating diabetes, it could be used to aid weight loss. How does it work? Semaglutide is a glucagon-like peptide-1 (GLP-1) receptor agonist – which simply means that it binds to the GLP-1 receptor to mimic the effects of the hormone. GLP-1 exists in multiple sites in the body and its existence in the pancreas is where semaglutide’s anti-diabetic properties come to the fore. The drug helps raise insulin levels, which type 2 diabetics struggle to do, and this in turn lowers blood sugar. But GLP-1 also exists in the brain, and some of its many properties include working to both delay food leaving the stomach and increase the feeling of fullness one usually has after eating. This is where its weight loss benefits come in.
To quickly dispel a common inaccuracy, it’s important to note that the NHS-approved semaglutide used for weight loss isn’t actually called Ozempic – this is the name for the diabetes medication. In the UK, Wegovy is the brand name given to the prescribed slimming aid. And to confuse things further, GLP-1 receptor agonists are not the only type of new weight loss medication that exists. Another drug tirzepatide (brand name Mounjaro) targets both GLP-1 and another hormone called gastric inhibitory polypeptide (GIP), which also acts to increase satiety.
In 2025, as rates of both diabetes and obesity continue to rise, almost 100 years of research into these multipurpose hormones – by scientists from around the world experimenting with, amongst other things, lizard venom – has brought us medications proven to be effective in treating both conditions. And Wegovy does work: the two-year STEP 5 trial found that people on the drug lost on average 15 per cent of their body weight, almost six times that of those taking the non-drug placebo.
So impressed is the Labour government by the semaglutide hype that Health Secretary Wes Streeting has even suggested weight loss jabs will help his party get people back to work. Meanwhile, pharmaceutical giant Eli Lilly is collaborating with the government to commit £280 million to tackling health problems including obesity. So: good news all round? Well, not quite.
58-year-old Susan McGowan struggled for years to control her weight. As excitement about the miracle-working properties of weight loss drugs grew, the Scottish nurse decided to give them a go. After researching Mounjaro, Susan made her first order via an online pharmacy. The medication is taken as a single-dose weekly injection; over two weeks, she injected the drug twice. Just days after her second injection, severe stomach pain forced Susan to go to hospital, where she died last year. Her death certificate listed multiple organ failure, septic shock and pancreatitis as causes. It also noted the use of tirzepatide as a contributing factor, making Susan’s the first death in the UK officially linked to the weight loss drug.
In Breeda’s inquest in Ireland this week, the coroner raised concerns over members of the public using weight loss medications without medical supervision. It’s an issue of concern in the UK too – particularly given the list of potential side effects of weight loss drugs is not short. Drug trials have found that around a fifth of semaglutide users experience nausea, one in ten struggle with diarrhoea and vomiting and others complain of ‘Ozempic face’ – when rapid weight loss causes your facial skin to sag. More concerning side effects range from stomach paralysis to depression, while longer-term complications can include pancreatitis, gallbladder disease and thyroid tumours.
There have been 18 deaths over the last four years flagged up to the country’s medications watchdog over fears they had links to slimming injections. The jabs were either being used jointly to treat diabetes or for weight loss alone. ‘People just think it’s a miracle injection and you get skinny. I don’t think people really are aware that it can cause long-term medical conditions,’ Lorna Edgar told ITV News, after she was left with chronic bowel problems and without a gallbladder when she developed pancreatitis on the drug.
In recent months, a flurry of first-person news pieces have lauded the miraculous effects of these new injections and NHS officials have applauded their weight-shedding potential – but concerns are growing under the surface. The National Institute of Clinical Excellence is currently carrying out a consultation on whether tirzepatide – the drug that Susan took – should be rolled out across NHS England. Officials stress that limitations are already in place, with Wegovy available for no more than two years from a specialist service and its use only recommended for those with an unhealthily high BMI. Yet there remains very limited scientific literature on the reasons why some users become extremely and rapidly unwell after using these jabs, and there is a lack of longitudinal studies on their long-term impact.
Not everyone is as hopeful as Streeting that Wegovy could bolster Britain’s workforce, either. Personal injury experts have concerns that the ‘long and short-term impacts of the weight loss jab could not only lead to sick days from the workplace’ and warned that the medications be ‘met with caution and not as a “quick fix”.’ Dietician Priya Tew told me the government has to be careful about its messaging on the matter: ‘Suggesting that people who are overweight or obese are unable to work… There’s this economic value placed upon it that is quite disturbing.’ And Dr Ellen Welch of Doctors’ Association UK also has doubts: ‘I worry the numbers don’t add up and GPs are going to be facing an overwhelming demand to prescribe without the resources to do so. We need to tackle the root cause of obesity and prevent it taking hold in the first place.’
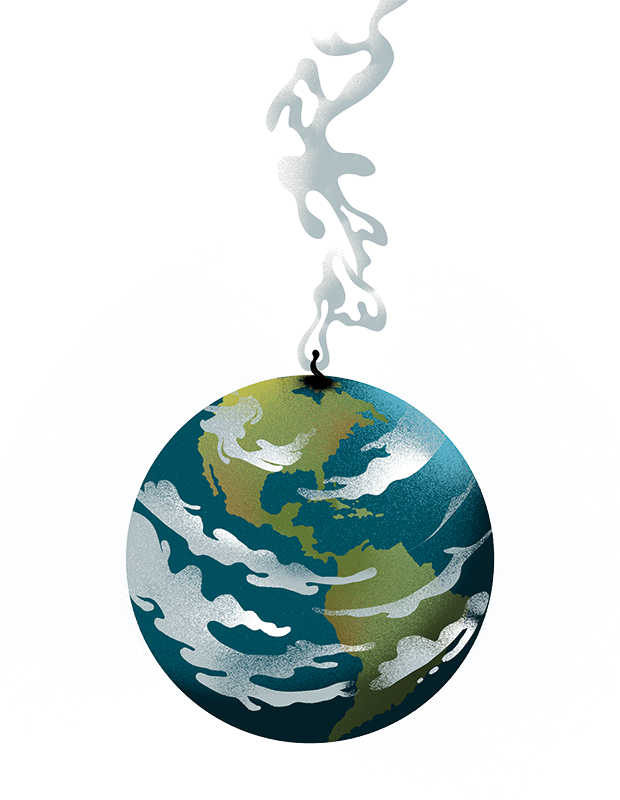
There is no doubt that the potential of these kinds of drugs to counter obesity, diabetes and possibly even Alzheimer’s is extremely exciting. And as one GP tells me: ‘Obesity is very dangerous in itself and it’s hard to argue we should stop using these drugs altogether.’ But if something sounds too good to be true, it probably is. We’re still in the early days of weight-loss jabs and a number of important questions about risk and outcome remain unanswered. While many in Britain’s political class were fast to dabble with the drugs – from Boris Johnson to Robert Jenrick – the government should be wary of seeing semaglutide as a quick fix. It may just be that Ozempic is not the wonder drug we think it is.








Comments