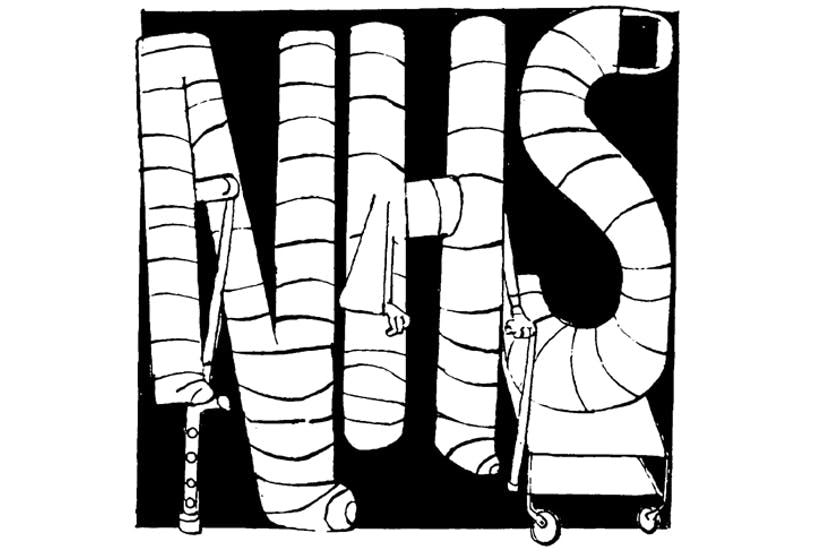
A week doesn’t go by without at least one horror story about the National Health Service hitting the headlines. But today you can take your pick. From the Institute for Fiscal Studies, which says the NHS will need £2,000 a year from each household to stay afloat, to the Care Quality Commission’s warning about patient safety in A&E, there’s a plethora of evidence that the NHS is on its last legs, and in desperate need of restructuring.
Many of the reports of the crisis in the NHS call for increased funding to compensate for the system’s underperformance. This week’s Spectator cover story reveals that Theresa May will be gifting the NHS the infamous pledge of £350 million per week extra by the next election as part of its 70th birthday next month. As James Forsyth and Fraser Nelson note, the cash boost is an undoubtably popular move. But as with all aspects of the modern-day healthcare debate in the UK, this change seems to reflect political considerations, not patient considerations.
Even if public spending on the NHS were to increase to the levels recommended today by the IFS or IPPR, it would still be the sick system of Europe, ranking in the bottom third of international comparisons for health system performance. According to the IFS, it will take a short-term increase of five per cent in annual spending to ‘enable waiting time targets to be met’. Perhaps this would be a selling point if Britain’s waiting times, even when met, weren’t some of the longest and most dangerous in the region.
It is not a matter of a bit more money to guarantee top-quality care. The system, which was not designed to cater to the needs of 65 million people and an ageing demographic, is falling apart under the pressure, unable to meet decent standards for the most basic and necessary services. A new survey of GPs released today, finds that 17 per cent said they had to turn down patients attempting to see a GP for a routine matter. Meanwhile, CQC reports that the:
“Quality and safety of urgent and emergency care remains a concern with 50 per cent of urgent and emergency services rated as requires improvement or inadequate overall and 8 per cent of services rated inadequate for safety.”
Exactly how much more tax are the British public expected to pay to cover up for a fundamentally broken healthcare system? Be assured, the extra cash is not coming from Brussels’ payments, nor is it going to be siphoned off from already existing, less meaningful government projects. It’s going to come from taxpayers, who – despite paying more for their care – will have as little say and control over their own healthcare provisions as they have now.
It is no great mystery why patient outcomes in the UK are on par with those in the Czech Republic, rather than those in Germany, Belgium, or Switzerland – and the answer isn’t simply more funding. While Britain has doubled down on its centralised system, which dictates healthcare policy from the top-down, its neighbours have put patient care at the heart of their agendas. The social health insurance systems in Europe allow for funding to go straight from the patient to the provider, creating more efficiency and better outcomes across the board.
If we are going to discuss additional funding for the NHS, let it be part of a wider discussion about redesigning a system that currently prioritises bureaucrats over patients. Otherwise, the failures of the NHS will still make the headlines. The only difference will be that the horror stories will be more costly, in every way imaginable.
Kate Andrews is news editor at the Institute of Economic Affairs





Comments