Labour’s plan to reform elective care is nothing new. Successive governments over the last twenty years have tried and tested reform in the NHS and the result is a minefield to navigate for both patients and staff alike. The resulting bureaucracy has left doctors and patients baffled.
The process can be mind-numbing and leaves doctors who just want to help patients despairing
It’s no surprise then that doctors like me are sceptical about the government’s planned shake-up which was unveiled by Health Secretary Wes Streeting last week. While the changes are designed to ‘empower’ patients, it’s likely to leave them even more confused.
The announcements include the expansion of ‘Community Diagnostic Centres’ (CDC), increased use of the NHS app, and control for patients to choose where to get their investigations and treatment from. But will these things provide a magic bullet to the NHS’s woes? It seems unlikely.
Take, for example, the case of Sarah, the fictional patient in the announcement (which has now been removed from the internet). Sarah visits her GP practice for sinus pain and hearing loss and is referred by a nurse practitioner for a CT scan at a new ‘CDC’. The results are fed back to her via the app, and the nurse will have a discussion with the consultant at an multidisciplinary meeting, where a decision is made for her rhinitis to be managed in the community, and further investigation is required for the hearing loss.
This is a lot of new steps introduced to a pathway which already would have likely got the diagnosis or referral in one consultation. In theory, if this patient attended their GP practice to see a doctor who could diagnose rhinitis, they could have been started on a trial of corticosteroids as per the current pathway and been referred to audiology for their hearing. This saves unnecessary appointments and radiation from scans which might not even be required. GPs are currently able to contact specialists, such as an ENT registrar, over the phone from their practice if they believe a patient warrants more serious investigation. We have a cohort of high standard generalists who are trained to make these decisions; switching the pathways by adding additional steps is pernicious, and judging by online response, there is a consensus between GPs and surgeons alike that this is a terrible idea.
The irony is that Streeting has made a case for the resurgence of primary care. The Health Secretary clearly understands its importance in dealing with the crisis in the NHS and seems eager to cut the fat of bureaucracy in the health service. It’s hard then to understand this policy, given the risk that it makes things more complex than it needs to be for both doctors and patients. In reality, patients want their local GP practice to be able to give them an appointment, and their local hospital to allow them to get the scan or procedure they need doing, something which is achievable already.
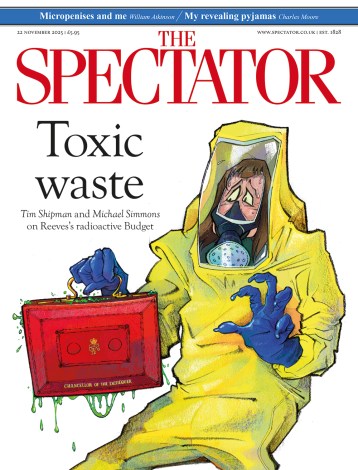
The use of the independent sector and increased surgical hubs is helpful but not quite the game-changing policy Keir Starmer – who has described it as ‘radical’ – seems to believe it to be. Previous Conservative administrations have, after all, been doing something similar for some time. While some of the latest changes are likely to improve short-term waiting lists, there is no clear direction out of this backlog for the long term. This seems in keeping with Starmer’s political ideology more generally.
Likewise, Labour seem to have ignored the crisis of staff shortages, which currently stand at over 100,000. You cannot bring down waiting lists without having more specialists, and yet low speciality training numbers for doctors are having a bottleneck effect, leaving many resident doctors unable to specialise for years on end. The 2024 competition ratios for training doctors revealed core surgical training to be 5.25 applications per place, over double what it was ten years earlier. This represents a failure from successive governments and is a reminder of how deeply flawed the NHS workforce plan is going forward. A sensible change would be to expand this along with the physical capacity of hospitals, increasing the number of specialised doctors able to perform the procedures required and giving more capacity to do so. This would also counter the looming problem of the rising number of doctors retiring who are able to do these procedures.
Another useful suggestion would be to have uniform IT systems for scans across all care. One of the most frustrating processes as a doctor is trying to call another hospital’s switchboard to get previous scans a patient has had available on the system. This information can be vital in diagnosing and treating a patient as it helps us rule out longer term potential cause. I can spend up to an hour on the phone sometimes, and three hours waiting for scans to download. It’s an experience which I am sure other clinicians can relate to. There are times where you are transferred from department to department over the phone, with no one able to understand where you are supposed to get the scans from. The process can be mind-numbing and leaves doctors who just want to help patients despairing. It is baffling that, in 2025, a time of artificial intelligence and wearable technology, the NHS has different IT systems across hospitals and practices. Why is accessing scans from another trust one of the most difficult tasks you will do as a doctor? It shouldn’t be this way.
Doctors can point to many other examples of inefficiencies plaguing everyday tasks in the NHS. These range from difficulties referring patients for follow-up appointments, trouble booking scans to the nightmare of getting a bike space in hospital lockers. It feels as if some tasks that should require one to two steps end up requiring seven. And while regulation and oversight is needed for safety in a healthcare system, the NHS feels so bogged down in this clutter it adds to the general atmosphere of malaise to what was once a revered service.
Labour came in promising change and reform, suggesting that otherwise the NHS would ‘die’. But the early indications are that their reform is weak and misguided and seems unlikely to provide any long-term benefit to patients or practitioners.





Comments