Britain has picked a fight with the pharma industry, and it isn’t clear why we think we can win. Not only might NHS costs rise, but we may also lose access to new medications, making our health service increasingly second class and meaning that people die. Health Secretary Wes Streeting’s fight has made headlines and negotiations over costs between pharmaceutical companies and the government have failed. Eli Lilly, for example, has paused British sales of their weight loss drug Mounjaro, and when they resume next month they will do so at almost triple the price.
Several threads tie the current problems together. The first is that governments and pharma companies are always arguing about prices. One represents taxpayers, the other shareholders; the interests of the two overlap but are not identical. Drug development and manufacture is fearsomely expensive and fearsomely regulated. That means the free market cannot be relied upon, and arguments are necessary and always will be.
Britain can no longer expect, as a small player in a global market, to make the rules
The second thread is that our existing deal has problems. Two decades ago, the government health body NICE plucked out some figures for what they thought represented value for money in healthcare. They decided that £25,000 to £30,000 per QALY (Quality Adjusted Life Year) seemed reasonable. A quango decided for themselves how much our lives were worth and, even in retrospect, did a good job.
NICE is a rare British institution whose achievements remain respected at home and admired abroad, but their figure for how much they’re willing to spend on buying drugs for the NHS has never changed. The value of my living room and socks has grown with inflation; NICE’s valuation of my life has not. As a result, companies increasingly aren’t bothering to ask for their new drugs to be approved in Britain. Asking pharma to stick to old prices is asking them to freeze time. Similarly, the VPAG scheme – the voluntary scheme for branded medicines pricing and access – caps their sales, with pharma actually paying us when the NHS buys more than a certain value of their drugs. The more we buy, the more they pay us: a deal beyond the dreams of modern shoplifters, and the opposite of how markets work.
Our government’s job is to fight our corner, and if they can manipulate the markets to favour us, we benefit. For a long time Britain has done a remarkably good job in this regard. Globally our share of the market is small, but NHS centralisation helped with bargaining power and we have got drugs at advantageous prices. That’s now changing because of the third thread: Donald Trump.
America has long been the largest market for pharmaceuticals and it has long paid the highest prices. Their healthcare costs a fortune, with everyone involved extracting value (or blood, depending on your perspective) at every point. Americans spend a vastly higher proportion of their GDP on healthcare, get poorer outcomes, and – a point you probably won’t share my pain over – have richer doctors.
Why, Trump’s government has asked, should the biggest market in the world not leverage its own bargaining power? Why should it not get a better deal for its own taxpayers? The answer is that they absolutely should, and what’s happening now is sensible for them even if it looks set to cost us. If pharma want to sell their drugs in America, Trump’s demanding they match the lowest prices they’re offering to other developed countries.
Pharma companies selling us drugs at reduced prices haven’t lost much by doing so because the British market isn’t huge. Going forward, if they reduce their prices for us, they have to reduce them for America – which comes at a far more serious cost. Our best hope is they advertise an expensive list price to keep the US happy, then actually sell at a huge discount. Everyone would know, but if the American civil service has pockets of incompetence to match our own, it could work. Why pharma should risk it, however, is less clear.
Drug costs ratchet upwards because of innovation. Each year, our arsenal of effective medicines gets bigger. That’s not an obviously soluble problem, nor an unwelcome one. Nor is it enough to say that pharma should sell more cheaply, although endlessly tinkering with intellectual property protection and financial rewards is essential – we want to be maximising that innovation by allowing profit, not maximising profit by allowing innovation.
Regulation around manufacturing drugs, whether brand name or generic, is stringent everywhere, as it should be, but vastly slow and expensive, which it needn’t be. Unable to keep up with demand, Novo Nordisk began building a new manufacturing plant for Wegovy in the US in 2024, as did Eli Lilly for Mounjaro. Despite their willingness to invest their vast sums, regulatory drag prevents pharmaceutical companies from setting up new manufacturing sites quickly – even though that would increase supply and pull down costs. Even regulation about packaging, for drugs whose manufacture has already been thoroughly regulated, adds needless millions and huge delays, raising prices not only for brand-name drugs but generics too. Everyone cares about caution, which they should, but few care about competence. The added costs are vast – and in no one’s interests save those whose jobs exist only to slow everything down.
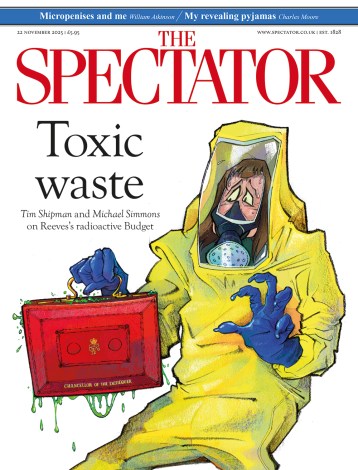
Squeezed between fossilised pricing models and the new reality of an America no longer willing to be taken for quite such a fool, Britain has a problem. Diminishing the self-inflicted harms of our incompetent regulatory sclerosis would help, but our ability to expect cheaper drug prices than the rest of the world looks finished. Streeting can win some easy publicity by lining up against Big Pharma and complaining of their profits but can no longer expect, as a small player in a global market, to make the rules. Special results can only come through being more nimble and efficient than other countries.
‘Death in old age is inevitable,’ said one of the greatest of last century’s doctors, Sir Richard Doll, ‘death before old age is not.’ Since the second world war, about half of our increase in healthy life has come from ever better drugs. We need them, and we are going to have to pay for them.






Comments