One in seven British adults – almost nine million people – now take antidepressants. Yet a study attached to the University of California San Francisco suggests we don’t actually know if they should. The paper from the US, led by William Ward and published last month, exposes a glaring flaw: American trials test these drugs for months, while in the real world patients take them for years. In the UK, for example, just over 25 per cent of patients have been taking antidepressants for five years. This gap raises a question medicine has faced before: how do we know our treatments work?
Antidepressant usage has soared but happiness has not
For centuries, doctors did more harm than good. Bloodletting was done because patients and doctors both believed they could see it working, overestimating their ability to see patterns in the storm of natural variation. They were wrong, but the lesson is not that people in the past were fools – rather that observation and experience of medical phenomena can be misleading. Only certain types of scientific experiments can distinguish truth amongst the variation and flux of human lives.
Randomised controlled trials are required. In the case of antidepressants, our randomised controlled trials are a mess. Most skip key questions – like what the optimal duration for taking them is or how to safely wean someone off them – and offer no solid evidence that long-term use helps more than it harms.
Worse, many trials offer only the false pretence of being reliable. They should compare their drug with a placebo, a fake pill designed to be indistinguishable. This means patients might be able to tell what they’re taking, making the appearance of a placebo control illusory. Stripping away the power of our prejudice is important even when dealing with phenomena that are strictly physical, like blockages in coronary arteries, and it’s critical when measuring something subjective like mood. Stopping antidepressants can feel terrible, but withdrawal may reflect dependence on the drug, not benefit. Vinay Prasad, Ward’s senior colleague on the new paper, notes that heavy drinkers who suddenly quit often then feel worse – but that doesn’t mean their drinking was good for them.
Medicine has long assumed treatments work without having sufficient proof, and history is full of doctors, even the most brilliant, prescribing treatments with absolute confidence – only to be disastrously wrong. Before high-quality reliable medical trials emerged after the second world war, many medical treatments weren’t just ineffective; they were harmful. Psychiatry is repeating these mistakes by failing to rigorously test when and how its treatments should be used.
When the first antibiotics were discovered, their effects were so dramatic that no structured experiments were needed to show they helped. Streptomycin, which came after penicillin, plainly helped with tuberculosis of the brain and spinal cord. Without the drug, everyone died; with it, many lived.
Most situations in medicine, though, are not like that. When tuberculosis affected the lungs, for example, many people died, but many recovered. Working out whether a drug helps in such a setting requires something better than just unaided experience.
Streptomycin, for example, was thought likely to help treat tuberculosis but was known to have brutal side effects. When George Orwell took it in a doomed attempt to treat his own disease, his nails fell out and the skin of his lips sloughed off; each morning he woke with his mouth glued shut by blood. Taking the drug, he wrote, was ‘rather like sinking the ship to get rid of the rats’. Only a randomised controlled trial of streptomycin was able to work out whether on balance the drug did more harm or good. The side effects of antidepressants are less dramatic, but they are real – ranging from gut problems and weight gain to a sex life stripped of joy. Working out whether the benefits are worthwhile is not easy.
Psychiatry in the first half of the 20th century focused on talking therapies. Post-penicillin, it embraced a different view of human life: one in which our moods were not reflections of our character and experience but attributed to predictable consequences of our biochemistry. Depression as a state of mind was abandoned in favour of seeing it as a molecular glitch, a preference psychiatry still clings to today. No coincidence that psychiatrists, who once favoured images of themselves as thoughtful listeners, now prefer posing with stethoscopes and scrubs.
Oddly, psychiatry clings to this model despite accepting that depression is not a simple chemical imbalance with an obvious pharmaceutical fix. Pop culture still equates serotonin to happiness, but science has dropped the notion that serotonin, or any single neurotransmitter, dictates our mood.
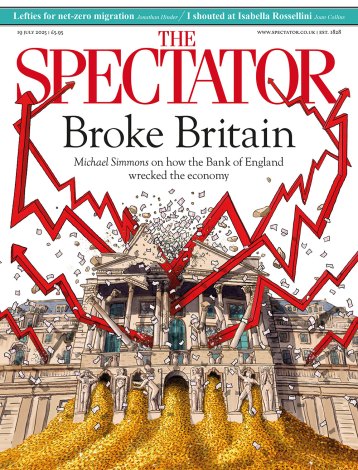
Depression and psychiatric labels have become a modern norm without seeming to help us or make us better off. Antidepressant usage has soared but happiness has not. Mental illness now strains our economy, with ever more spent supporting those who cannot work, or who cannot work fully, or who can work but struggle to live.
A friend, thoughtful and observant and insightful, told me that without a 10mg white pill every morning for four years he believes he would have failed. I trust his experience – but not that he can untangle the effects of the drug from that of placebo, or know if four years was too long.
No question that mental health is a complex problem. But for every complex problem, as the journalist H. L. Mencken noted, there is a solution that is simple, neat, and wrong. Pills for low spirits may be today’s perfect example. Those who falter, struggle, or sense they might fail deserve to be taken more seriously. Until psychiatry embraces rigorous, long-term trials, it gambles with millions of lives. And history is clear that when medical science bets on bad evidence, patients lose.






Comments