Self-testing is now available to any individual wishing to rule out conditions such as diabetes, pregnancy and bowel cancer.
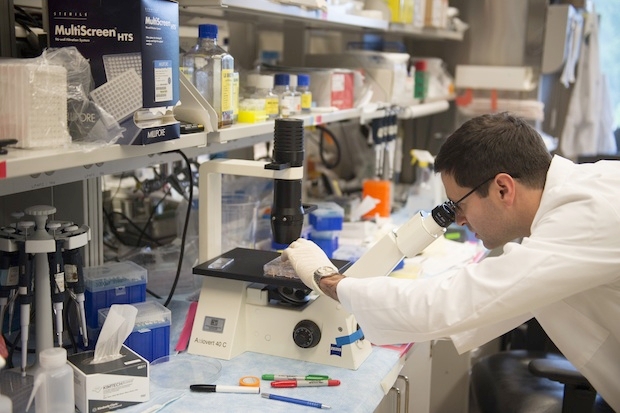
Traditionally, however, screening for cervical cancer has required women to attend a GP surgery in order to have a small sample of cells scraped from the surface of their cervix by a doctor or a nurse. The sample is then sent to a laboratory to assess the cervical cells for any abnormalities (cytology testing) and/or to test for human papilloma virus (HPV) DNA. Some types of HPV may cause cervical abnormalities that can subsequently go on to develop into cervical cancer. Several studies over the past decade have also demonstrated the superiority of HPV DNA testing over cytology.
Around 20 per cent of women do not attend cervical screening for a number of reasons including, for example, difficulties relating to travel, childcare, work commitments and problems in accessing screening at an appropriate time and place. Others are put off by the potential embarrassment and discomfort of the whole process.
But all that could be about to change. Important work undertaken in both China and Mexico over recent years has highlighted the potential of self-sampling for HPV DNA. In some recently published research on 100,242 Mexican women aged 25-75 and from low-income backgrounds, 11% (10,863) self-tested positive for HPV DNA.
In a study due to be completed later this month women attending five surgeries in London have been offered the option of self-testing for HPV using a swab. The self-sampling can be undertaken at the individual’s home as opposed to at the GP surgery.
In addition a separate analysis of 36 studies comparing the accuracy of HPV DNA testing on self-collected samples in comparison to clinician-collected samples has been published. Form this it seems that self-sampling can be as good as sampling by a doctor or a nurse if the subsequent DNA analytical method is of a sufficiently high quality.
Cervical cancer remains the most common cancer in women under the age of 35 years and the last decade has seen an increase in rates amongst younger women. Perhaps offering more convenient and acceptable approaches to cervical screening might help to reverse this trend.




Comments