Party conferences are less about conferring than about speeches and announcements. Today Keir Starmer revealed NHS Online, a virtual hospital of vast scope and wonderful promise. Patients will be able to swiftly connect to clinicians at a time and place to suit them. NHS Online, said Starmer, demonstrates that Labour favours ‘renewal’, while Reform only pursues the ‘politics of grievance’.
Grievance is a miserable trade. Presumably it wasn’t grievance that led Starmer to call Reform’s policies racist and their supporters – if not racist themselves – too stupid to understand what they were backing. Insulting Reform voters is always likely to land well at the Labour party conference, although it’s not an obvious route to winning those voters back. But making the NHS better should be safer ground for both, and NHS Online aims to do just that. ‘A new chapter in the story of our NHS, harnessing the future, patients in control. Waiting times cut for every single person in this country.’ Starmer’s speech is so rhetorically bold as to brush past normal requirements for finite verbs and sentence structure, but it also ignores practical details. They matter.
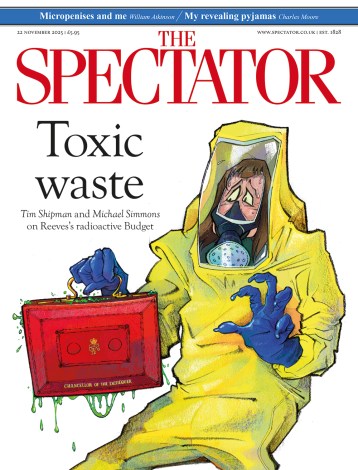
Human contact has a value that video links can’t carry
Strange that NHS Online – due to be in use from 2027 and offering 8.5 million appointments in its first three years – wasn’t foreseen in the NHS ten-year plan, all of two months ago. Cynics – if there can be any left, given Starmer’s achievements since he announced ‘phase two of my government’ a month ago – might wonder if the government is making things up as it goes along, without serious thought, just to have a conference announcement.
There are odd facets to the announcement of NHS Online. Trusts already offer virtual appointments – they have been popular since Covid, possibly with doctors more than patients. Offloading them to a virtual institution, in both the press release and in Starmer’s speech, seems full of possibility. Geographical proximity will become irrelevant; patients will be able to book follow-up scans, procedures, and appointments wherever they wish.
The potential benefits are real, but so are those of having virtual appointments with people connected to a local, physical system. Replacing that with NHS Online means turning care over to an unproven national IT project, commissioned, developed, and run by the government and the NHS. If that doesn’t chill you, it should. It chills me, because I use NHS IT for my daily work.
A key issue, which worryingly seems entirely overlooked in the speech and the press releases, is inter-connected IT. Clinicians using NHS Online need to see your records or they won’t be either safe or helpful. No one has ever solved the inter-operability problem within the NHS, with different computer systems that can’t communicate with each other. Over £10 billion was squandered on the NHS’s National Programme for IT before it was scrapped; billions more have gone the same way on care.data and other abandoned rollouts. Liz Kendall’s promise that UK ‘tech sisters’ will challenge Silicon Valley’s tech bros hardly inspires confidence that the problem will be solved – or even recognised.
Beyond the technical challenges are difficult questions about what can and can’t be done online. The questions are difficult because underpinning them is the thorny subject of what it is that doctors actually do.
This is more elusive than it looks; after thirty years in hospitals, it isn’t clear to me. Proponents of AI have long predicted doctors’ redundancy. Geoffrey Hinton, whose work on machine learning won him the nickname of AI’s Godfather, as well as a Nobel, said we should stop training radiologists because their skills would be redundant within five years. That was in 2016, and today there is a global shortage of radiologists – not because we stopped training them, but because their skills are more in demand than ever.
Proponents of AI tend to make the same mistake as devotees of hospital dramas, believing that doctors are there to make clever diagnoses. There are doctors who like to pretend the same, but they know they’re pretending. Rare cases provide a challenge; most do not. When I was part of a team of A&E doctors, we used to play a game, on quiet shifts, of guessing the diagnosis as people walked in, or were wheeled in by paramedics. We were usually right.
A grey haired colleague once said medicine was a faith, hospitals its temples, and doctors its high priests. Fanciful, but it captured a truth: human contact has a value that video links can’t carry, even if they have carefully chosen backgrounds. A physical examination is a laying on of hands. Certainly reassurance is a central part of what we supply, and it isn’t always even reassurance that everything is going to be ok. I have been called to scenes of panic and terror and been able to helpfully explain that all that is happening is death. People calm down. The terror is often not knowing if you should be doing something, or if there’s something that needs doing. A doctor’s role is often to contain people’s anxiety, or share their sorrow.
Part of what doctors and nurses do can be replaced by computers, or delivered digitally, although whether British governments can solve the technical problems that lie in the way is dubious. Clinicians must not resist change, nor behave like train drivers, blocking automation that would make them redundant. Some forms of human connection cannot be digitised. Conference-driven policymaking that mistakes press releases for progress is dangerous.






Comments