As someone who has lived with kidney cancer for many years, I have already addressed many of the questions others are having to ask themselves in light of coronavirus: What exactly is CPR? When should it be attempted? What do different life-prolonging treatments entail? What is their likelihood of success?
All of a sudden these questions are up for public comment and debate. And rightly so, we desperately need a frank, grown-up conversation about how we die, not just how to plan our funeral. Coronavirus may well change the way we talk about death and dying for good.
But the majority of the discussions I’ve seen play out over recent weeks have not involved those of us with life limiting and terminal illnesses. This is particularly galling when questions arise about when treatment should be refused, who should make these decisions and what a good death should look like. Surely we are in the strongest position to answer them?
For us, these quandaries are not hypothetical; they are our lives. Yet at times we can feel silenced and sidelined in public debates about death, trapped between two extremes of paternalism: one which seeks to control the choices we make as we die – particularly if we don’t want to fight off death at all costs – and another which pats us on the head and calls us ‘brave’ for even acknowledging the unavoidable fact that we are dying.
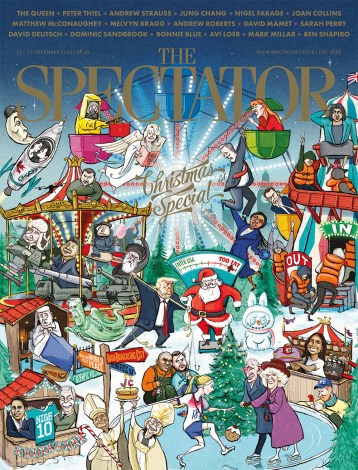
Last week, an article in The Spectator inferred that people who want to refuse all life-prolonging treatment in the future using an Advance Decision (also known as a living will) could not possibly be qualified to make such a judgement. This idea, that you can make some decisions but only if they meet someone else’s moral standards, is still pervasive in medicine and it is the antithesis of truly personalised end of life care. The only person who should be able to ultimately decide whether I consent to or refuse treatment is me. How could anyone else possibly know the point at which I would find my quality of life intolerable?
When I was first diagnosed with renal cell carcinoma, I had one of my kidneys removed. Several years on, a tumour appeared on my adrenal gland on the original side and later two further tumours appeared on my remaining kidney on the other side. I was faced with major surgery and the possibility of dialysis. I felt some pressure from my medical team to do battle and not wave the white flag too soon. But neither option was curative, and I feared that waging war with my body could result in the loss of good time.
After careful deliberation I decided to jump off the medical treadmill and refuse any further tests or treatment, other than to keep me comfortable. I wanted to live, not endure. I redefined hope as hope for a good life, not the longest. Because ‘no treatment’ hadn’t previously been an option on the table, I worried that I would be pressured by my doctors to opt for the surgery, and decided to clarify my thoughts in a letter to them.
Later, with the help of my local hospice and the charity Compassion in Dying, I drew up a DNAR to refuse CPR and an Advance Decision to refuse all other life-prolonging treatments in future, giving further weight to my wishes. It had been an uphill struggle to make my voice heard and my wishes understood.
At the other end of the spectrum, people with life-limiting conditions can feel patronised for even broaching the subject of death, let alone openly discussing their decision to confront and plan for it. On Radio 4’s Any Questions a few weeks ago, a caller in her 80s with various health conditions who had a DNAR and Advance Decision in place asked how else she can ensure her wish to remain at home with end of life care is followed if she contracts covid-19. She was called ‘brave’ several times and the conversation quickly moved on to isolation measures, her question ignored. On Woman’s Hour more recently, hushed tones and euphemisms were adopted as soon as the topic of advance care planning – the process of considering and recording your end of life wishes – was raised.
It shouldn’t be seen as an extraordinary or courageous to face the inevitable. We need to stop calling them ‘difficult’ conversations. They are ‘important’ ones, and it’s not brave to have them, just sensible.
What people with serious health conditions do not need are commentators passing judgment on our own uniquely personal decisions, particularly if we prioritise a good life over a long one. Nor do we need pats on the head, whispered euphemisms and hurried changes of subject. What we need is to be respected as individuals with our own goals, fears, values and experiences, and to be trusted as having a valid opinion on what is best for us. If this pandemic does change how we talk about death and dying, and I hope it does, we must make sure all voices are heard.
Molly Bartlett is 73 and has lived with incurable kidney cancer for 20 years





Comments