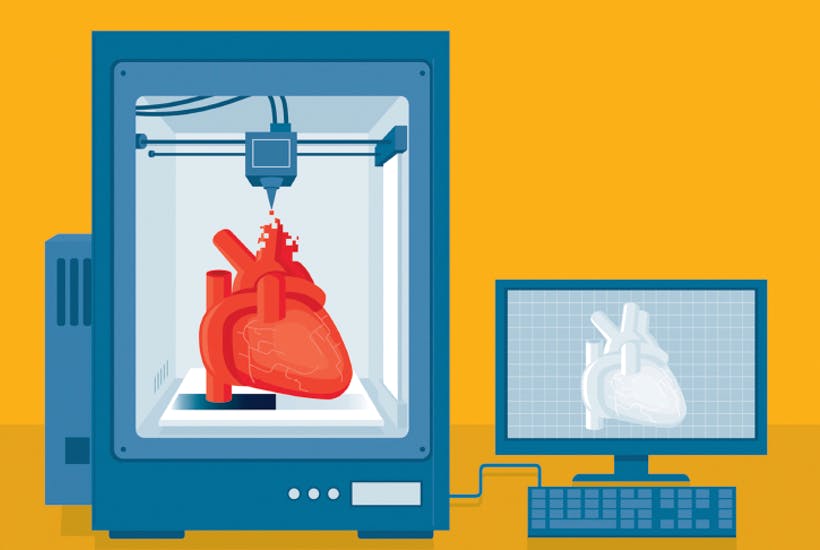
When The Six Million Dollar Man hit the world’s TV screens in 1973, few could have foretold how swiftly his sci-fi-inspired bionic implants might become reality. Yet 40-odd years later, the idea of creating perfect body parts through 3D printing (also known as additive manufacturing) and rebuilding humans from the inside exceeds all possible imagining. The benefits for doctors and hospitals are huge, but there are surprising low-tech advantages in other areas of healthcare, too.
At its most cutting edge in the laboratory, scientists are exploring bioprinting: the creation via a 3D process of organs which will become living tissue suitable for transplant. Bioprinted tissue has already been developed for research and the first transplantable examples could be ready for use in just a few years’ time. Sichuan Revotek, a biotechnology company based in Chengdu, China, implanted a printed section of artery into a monkey last year.
But additive manufacturing is most commonly associated with prosthetics: in dentistry, where 3D printing creates customised crowns, bridges and braces; or orthopaedics, where surgeons are now accustomed to using 3D printed joints in knee replacements. Off-the-shelf implants are still most common and offer perfectly good results for most patients. But Joyti Saksena, a consultant hip, knee and sports specialist at Total Orthopaedics in Highgate Hospital, London, says using 3D printing to create bespoke joints has been a godsend for more difficult cases.
‘Some patients may have a leg length discrepancy, or hips that have abnormal rotation or abnormal anatomy because of congenital or traumatic reasons,’ he says. ‘We can get good results with a standard hip replacement, but using a system like the Symbios HipPlan means we can rely on computer-aided planning to design and manufacture a hip which fits exactly to the patient. It’s about restoring their normal anatomy, as opposed to trying to make an implant fit.’
The pre-op work also means theatre time is reduced, saving hospitals money. ‘At the moment they are more expensive per implant, by and large,’ says Mr Saksena. ‘But savings in time and efficiency may offset that. At some point, printed joints will become far cheaper.’
In the oncology department, as well as being used for research purposes, 3D printing is transforming operations. In New York last month, Penelope Heller, a 20-year-old American with bone cancer, was given an entirely new titanium sternum and rib cage conceived and printed in 3D. Meanwhile breast cancer patients in South Africa are benefiting from the work of mechanical engineer Nneile Nkholise, who has developed breast prostheses for women who undergo mastectomies.
Dr Bissan Al-Lazikani, head of data science at the Institute of Cancer Research in London says: ‘Exciting uses span the 3D printing of organ scaffolds, helping model and direct therapy through the complex organs within the human body, visualise data in ways more accessible to the human brain and even support everyday lab experiments.’
One project she cites is AbdoMan, a 3D-printed human torso created by a team from the institute and the Royal Marsden NHS Foundation Trust. This replicates the uptake of radioactivity in the abdomen during radiotherapy. It’s already being used to measure how much radiation is being delivered to tumour models using state-of-the-art imaging techniques and will help to assess the effects of molecular radiotherapies in patients undergoing clinical trials.
Dr Al-Lazikani adds: ‘We are starting to use 3D printed models of our molecules to help us understand, for example, how drugs act to block the action of cancer-causing proteins. Finally, a more mundane use, perhaps, but likely to become ubiquitous in the not-too-distant future, is producing 3D-printed laboratory implements or instrument parts accurately, cheaply, rapidly and on-demand, along with the ability to adapt these instruments and make them ‘bespoke’ at no extra cost.’
Hospitals are also using 3D models in training and to plan and practise operations in advance, says Scott Radar, general manager of Healthcare Solutions at Stratasys, a leading 3D printing manufacturer. ‘This offers many benefits potentially reducing complications and the amount of time patients spend on the operating table, improving the success rate.’
Stratasys technology is being used in many areas of medicine: Mr Radar points to work at the University of Michigan as one exciting example. In 2012, doctors helped a baby born with tracheo/bronchomalacia (no cartilage in the windpipe) by creating a 3D-printed scaffold of absorbable material to help the body heal itself.
The technology is also useful when it comes to reassuring patients and their loved ones. Pankaj Chandak, transplant surgical registrar at Guy’s and St Thomas’ NHS Foundation Trust, where 3D printing was pioneered in paediatric kidney transplants, says it helps the public understand complex medical procedures. ‘We don’t only use models of the child’s abdomen for surgical planning,’ he says, ‘We also show it to parents to explain the operation. It is a better way to do this than drawing up diagrams.
‘There is nothing like having a 3D model to work with beforehand or with you during surgery for tactile interaction. It gives everyone involved more confidence.’
Dr Dianna Bardo agrees. A paediatric radiologist at Phoenix Children’s Hospital in Arizona, she helps prepare physicians for complex procedures by creating accurate models of defective hearts, limb deficiencies, injured internal organs, and even tumours using the Cardiac 3D Print Lab, 3D printing and advanced post-processing technologies of images from Philips Systems.
‘When I model that tumour or model that heart or bone into a three-dimensional object in our 3D lab, it’s an instant picture,’ she says. ‘It’s something anybody can perceive.’




Comments