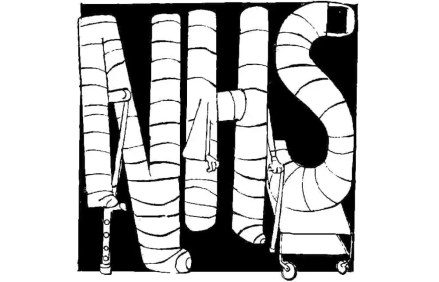
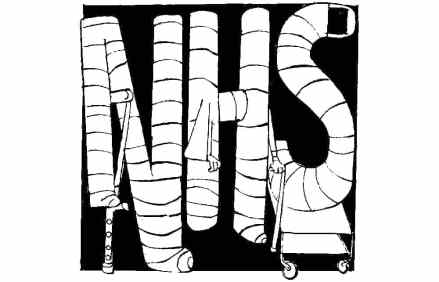
I want to see a doctor – not do another NHS survey
Nye Bevan did not make old bones, and perhaps that’s just as well. According to a recent British Social Attitudes survey, 52 per cent of those polled are dissatisfied with the NHS, in particular with the difficulties in getting a GP appointment, with long A&E trolley waits and with huge delays for hospital appointments. All this, in spite of ever more money being chucked into its maw. If invited, I could immediately save the NHS a packet by dialling down the thermostat that has turned hospitals into Hotel Tropicana for bacteria, and by asking, wherever possible, patients’ relatives to provide food, thereby reducing the amount of unappetising slop that goes