Meet the bloated, useless General Medical Council
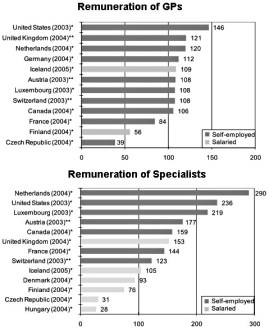
There was a time, not long ago, when British GPs provided the best home doctor service in the world. Patients could telephone their doctor 24 hours a day, seven days a week (including Christmas), ask for a home visit and get one. Patients prepared to visit the surgery could expect to see a doctor the day they called. Today, it is easier to find a plumber than a doctor at night and weekends. Patients wanting emergency help out of office hours must visit their nearest major hospital and spend hours queuing in the A&E department. In some areas the target waiting time is 12 hours, though in practice, things are