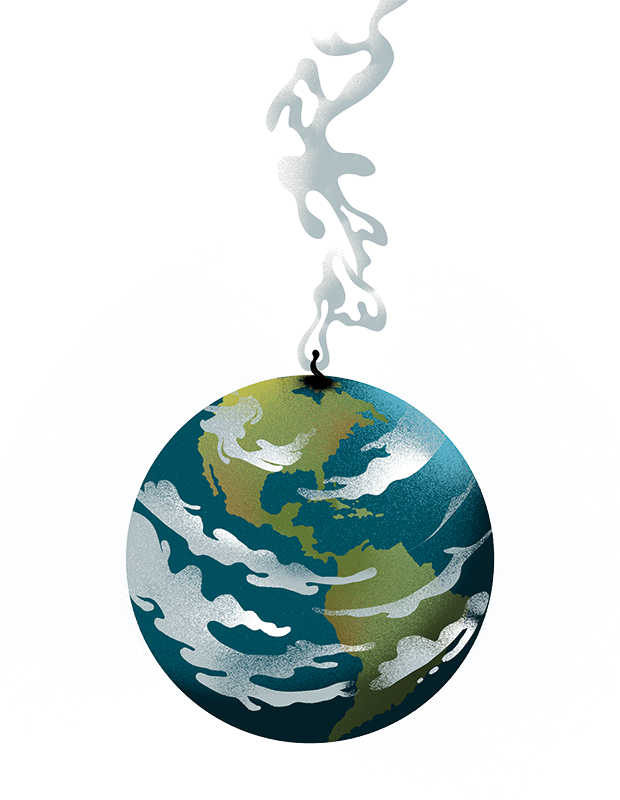
The Department for Health has published new performance league tables today which show that four in five NHS hospital trusts are failing, either because they are running substantial deficits or they are not meeting their performance targets.
The real reason that NHS trusts in cities like London perform better is the same reason that accountancy firms and legal practices perform better in London – they attract the highest quality staff
These league tables are the first of their kind to be published and were brought in by Wes Streeting with the aim of improving performance. Trusts which do well will be rewarded with bonuses and more freedom to decide how to spend their resources, whilst leaders of trusts which consistently fail to improve will have their salaries frozen.
The league tables match what most health policy experts would expect. Hospitals in the south-east of England, particularly in cities such as London, are doing very well, whilst hospitals in the north and west of England, particularly in rural areas, are doing much worse. This trend was already visible from the findings of the Care Quality Commission and the NHS oversight framework, which gives NHS organisations a score between one and four (where one is best).
Attempting to address this gap in performance between the wealthy south-east and the rest of the country has been a focus of the NHS for decades now. As early as 1976, the then-Health Secretary Barbara Castle set up a working party within the NHS to distribute resources away from the south-east. Another attempt to fix the imbalance was through ‘Golden Hellos’ for GPs to get them to work in underserved areas.
Similarly, Wes Streeting’s league table system is intended to be geographically redistributive when it comes to talent. Streeting will offer incentives for leadership teams in high-performing trusts to relocate to failing ones. This assumes that NHS leaders will be able to have a meaningful impact on performance – even though an executive team at a large hospital may be made up of fewer than 20 people with over 15,000 staff working beneath them. Their ability to change processes is often limited by a vast swathe of legal blocks and powerful union bodies.
But apart from anything else, the idea that these regional inequalities exist because of poor leadership is a case of putting the cart before the horse. The real reason that NHS trusts in cities like London perform better is the same reason that accountancy firms and legal practices perform better in London – they attract the highest quality staff. Sixty per cent of top achievers at GCSEs outside of London leave their hometown by the age of 32, with 30 per cent of that cohort moving to London, according to the Institute for Fiscal studies. It is just a fact of life that the majority of high achievers prefer to live in a global city like London with all of the opportunities it brings. Any top-down attempt to redress the problems caused by this imbalance without understanding its root cause is doomed to fail. Opportunities can be spread by executive fiat, but the talent won’t spread with it.
Not that it hasn’t stopped the NHS from trying. Beginning in 2024, doctors in training have been moved onto a ‘random allocation system’ for their placements as junior doctors once they graduate from medical school. In the old system, students who achieved the best marks were given their choice of where to train, with the best invariably choosing to live in major cities and the south-east. This system was introduced as part of a wider overhaul to address workforce gaps by redistributing junior doctors to remote coastal areas. Another reason that random allocation was introduced was because critics of the system pointed out that the worst performing medical graduates were disproportionately ethnic minorities and those from ‘disadvantaged backgrounds’. Even so, rather than fixing the NHS's regional disparties, random allocation is just demoralising the best performing junior doctors and making them more likely to quit the profession entirely.
The moment when a high-flying graduate is instructed to spend the next two years of their life living in a small village serviced by one bus per Saturday instead of a thriving metropolis – which they could have easily accomplished if they had chosen a career in the private sector – has its causes in a pathology of modern policymaking: an ultimately doomed desperation to achieve equal outcomes, no matter the human cost.







Comments