Every doctor can remember a time when bacterial infection laid waste to their patient with hair-raising speed and virulence. The most indelible for me occurred a decade ago during surgical night shifts. Again and again I was called to the bedside of a young woman with the ‘flesh-eating bug’, or necrotising fasciitis. By the time she’d presented to A&E, a recent graze to her leg was causing such disproportionate pain that her family had been forced to carry her. When the surgeons opened up the limb, they found carnage. Group A streptococcus – a bacterium that benignly colonises the throats and skin of millions of us – had burrowed from the graze into the deepest tissues, where it dissolved flesh with the ease of battery acid. Not even the most heroic operations could save her, let alone anti-biotics. Great swathes of thigh and pelvis were amputated in a series of ever more desperate surgical debridements to try to get ahead of the infection. By the end of the second night, the young woman was dead.
The maiming and killing power of bacteria hangs darkly over every page of Dangerous Miracle. This riveting book by Dr Liam Shaw, a computational biologist at the University of Bristol, has the essential hallmarks of all good science writing: boundless enthusiasm, ingenious metaphors and the effortless distillation of complex ideas into crisp, clean prose. Shaw presents the rise and fall of antibiotics – arguably the single greatest medical advance of the 20th century – as a ‘thoroughly modern story of technological hubris’. It’s impossible to disagree.
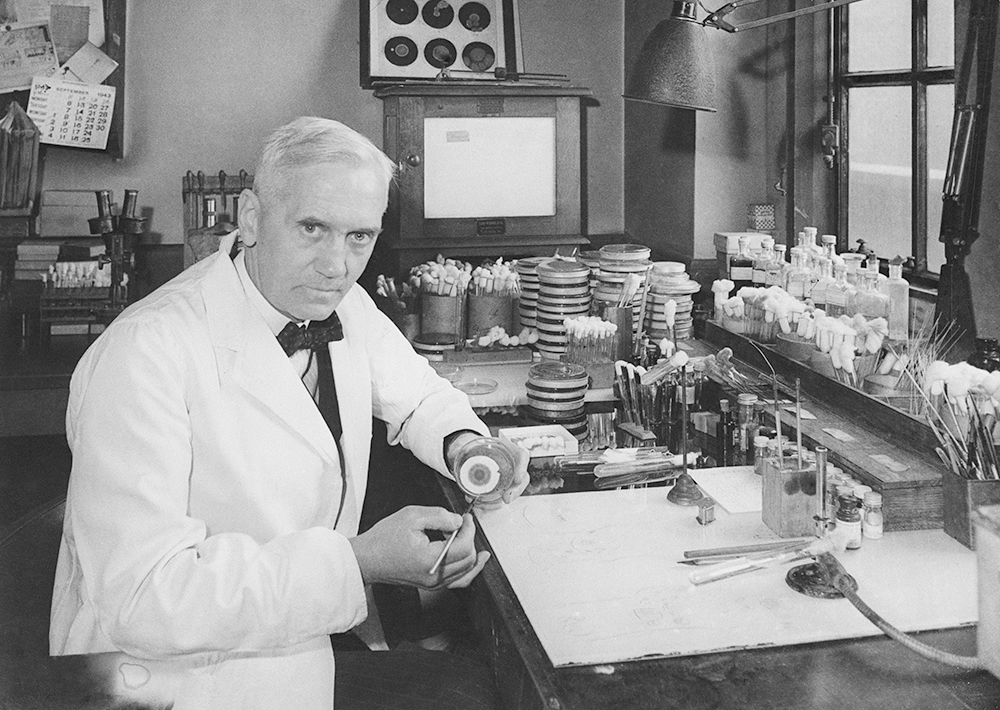
First, the decades of toil and tenacity. In 1928, the British bacteriologist Alexander Fleming discovered that a spore of the Penicillium fungus, drifting by chance on to a petri dish in his London lab, had mysteriously eradicated the staphylococci bacteria he grew there. He realised that a substance produced by the fungus – he called it penicillin – had the miraculous property of killing bacteria. Having worked as a field doctor in the first world war, Fleming had witnessed the gruesome effects of bacteria. Soldiers risked an agonising death by putrefaction once bacteria had torn through the skin’s barrier. As Shaw puts it: ‘In war, people kill people and bacteria take care of the rest.’
Fleming strove in vain to extract penicillin from the ‘mould juice’, and it took the advent of the second world war to galvanise the efforts needed to produce the drug in therapeutic quantities. In Oxford, fungal gloop was feverishly brewed using milk churns, copper cooling coils, a steel bathtub, a bronze letter box and even an old bookcase scavenged from the Bodleian Library. Obtaining one daily dose of penicillin – about 60 milligrams – required fermenting about 70 litres of raw broth. At last, in February 1941, penicillin was administered to a policeman who was ‘oozing pus everywhere’ from wounds sustained in a German bombing raid. The entire global supply of penicillin was used in one go – but it worked.
The first antibiotics were gleefully pumped into toothpaste, nasal sprays, shaving balm and even animal feed
Once the value of penicillin for treating injured soldiers was clear, the US government instigated a ‘race against death’. Fleming’s strain of Penicillium mould was flown in suitcases to the Midwest, where microbiologists and agricultural scientists joined forces to refine production. By the end of the war, a drug that had once been so scarce it was worth 250 times as much as gold was saving thousands of soldiers’ lives. Penicillin, a miracle of human ingenuity, had triggered ‘a transformation in human history without precedent. Within just a few decades, the world’s worst infectious diseases could be cured’.
But there was a catch. Almost as quickly as microbiologists unearthed more antibiotics from fungus in soil, doctors discovered they didn’t work for every patient. Certain strains of bacteria produced chemicals that enabled them to resist attack. The more that anti-biotic use killed the susceptible bacteria, the more the resistant bugs could thrive and spread, meaning the powers of the magic bullets waned over time. As early as 1954, a British doctor speculated that the proliferation of antibiotics might prove their downfall: ‘We may run clean out of effective ammunition. Then how the bacteria and moulds will lord it!’
This is, Shaw warns, the alarming state which humanity is fast approaching. Anti-biotic resistance has become one of the world’s most urgent global health threats. Already it is responsible for more than a million deaths each year – of people who should have survived had their infection been susceptible to treatment. In part, the problem is overuse. The first antibiotics were marketed as a panacea and gleefully pumped into almost every product imaginable: toothpaste, nasal sprays, shaving balm and even animal feed. Drug companies scoured the planet for the most obscure samples of soil possible, hoping to find the next penicillin in one of them. Pfizer recruited Arthur Sackler – of Oxycontin infamy – to help them sell their new drug Terramycin by pitching it as the world’s first ‘broad spectrum antibiotic’. (It wasn’t. It was almost identical to another new drug already on the market, Streptomycin, but the truth never stopped Sackler.)
Today, the system of patents that is meant to incentivise pharmaceutical companies to develop new drugs actively deters them from investing in antibiotics. Why pump money into a drug that is usually taken for only a few days when there are billions to be made from common chronic conditions such as diabetes or obesity? What is needed, as one pharmaceutical developer is quoted as saying, is recognition that antibiotics, unlike other drugs, are the
fire extinguishers of medicine. Imagine if the manufacturers of fire extinguishers only made money when one of their products was used to put out a fire. That would be absurd. But that is the situation for antibiotics: pharmaceutical companies only profit if they are prescribed.
Shaw concludes with a call to arms. Unless we want to return to an age when bacterial infections were a frequent death sentence, we need radical responses to this market failure. For, like fire extinguishers, the value of new antibiotics lies in their availability, not in their use. They need to be there in the event of a crisis – the emergence of a bug against which nothing else works. So should they be funded differently, through a subscription model, for example, as opposed to a fee each time a dose is purchased from a drug company? Or could governments collaborate to develop new antibiotics together – acting in the common good, just as they have done with the International Space Station?
These are fascinating ideas in need of urgent attention. In combining the passion of Robert Macfarlane with the incisiveness of Patrick Radden Keefe, Shaw has announced himself as a brilliant new voice in science writing.







Comments